Infirmité motrice cérébrale : ce à quoi il faut s'attendre
La vie avec la paralysie cérébrale
Qu'est-ce que la parésie cérébrale ?
L'infirmité motrice cérébrale, la paralysie cérébrale, la diplégie spastique infantile ou la IMC en abrégé est une lésion cérébrale qui se produit à un âge précoce, autour de la naissance, et constitue la cause la plus fréquente de troubles du mouvement chez les enfants. La paralysie cérébrale affecte principalement la mobilité, en fonction de la localisation de la lésion. Lorsque la marche ou d'autres mouvements deviennent difficiles, cela affecte la vie quotidienne de la famille. Il est donc important de soutenir ce développement moteur le plus tôt possible avec des aides appropriées et de maîtriser ensemble la vie quotidienne avec la IMC.
Lisez ici comment l'infirmité motrice cérébrale peut affecter votre enfant et comment vous pouvez soutenir de manière ciblée les mouvements de votre enfant.
Quelles sont les causes de l'infirmité motrice cérébrale ?
Il reste difficile pour les médecins d'en déterminer la cause exacte. En fait, il est souvent impossible de déterminer la cause ou les facteurs de risque d'une lésion cérébrale précoce. Les médecins cherchent également à savoir si de multiples facteurs peuvent être impliqués dans l'apparition de l'infirmité motrice cérébrale.
La cause est difficile à déterminer, mais voici ce que nous savons:
The known causes of cerebral palsy in children are very diverse. Doctors usually classify the causes according to the time at which children acquire the brain injury:
More than 50 percent are affected before birth (prenatal) or during pregnancy as a result of infection or lack of oxygen, for example when a blood clot (thrombosis) forms in a blood vessel in the brain and obstructs blood flow.
During birth (perinatal): From lack of oxygen at birth, for example.
Less commonly after birth (postnatal) as a result of infection such as meningitis or kernicterus, or overlooked rhesus incompatibility.

Les médecins trouvent de plus en plus de causes génétiques à la paralysie cérébrale et parlent de mutations "de-novo". Il s'agit d'anomalies chromosomiques qui peuvent être héritées, ce qui expose souvent les frères et sœurs à un risque accru de paralysie cérébrale. En outre, un certain nombre d'autres facteurs peuvent augmenter le risque de paralysie cérébrale chez votre enfant. Certains de ces facteurs sont les suivants:
les grossesses multiples
L'obésité de la mère pendant la grossesse
Les maladies infectieuses telles que la toxoplasmose ou la rubéole, ou les maladies causées par le cytomégalovirus ou le virus de l'herpès simplex avant ou après la naissance.
Les autres causes d'infirmité motrice cérébrale sont les suivantes :
Naissance prématurée : les enfants nés avant 28 semaines ont un risque accru de paralysie cérébrale.
Complications à la naissance
Poids de naissance trop élevé ou trop faible

Comment l'infirmité motrice cérébrale affecte-t-elle le développement de mon enfant ?
Chez les enfants, l'infirmité motrice cérébrale affecte généralement les capacités motrices ou la mobilité. Elle s'accompagne également d'autres symptômes tels que la douleur ou les troubles cognitifs ; certains enfants peuvent avoir des difficultés à parler ou à rire. Les symptômes dépendent de la zone spécifique du cerveau affectée, de sorte que tous les enfants ne présentent pas les mêmes symptômes et avec la même gravité.
Les signes suivants d'infirmité motrice cérébrale se manifestent seuls ou en combinaison:
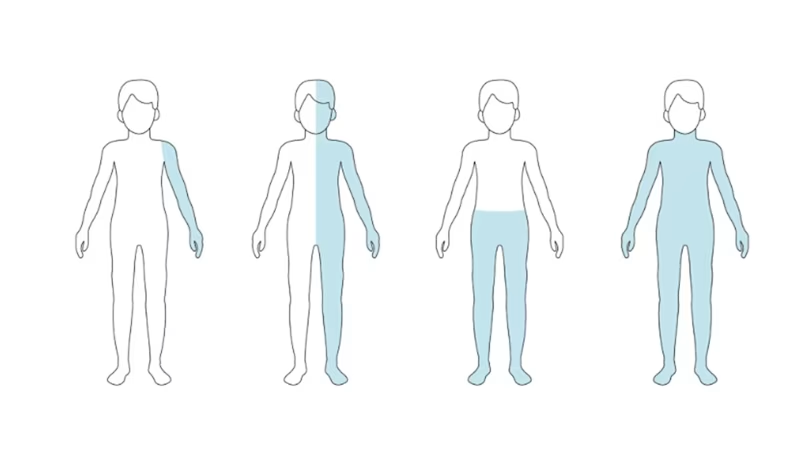
Based on the individual symptoms, doctors can distinguish between different types or classifications of cerebral palsy. The following overview shows the form of cerebral palsy behind the medical terms:
Understanding Infantile Cerebral Palsy
Infantile cerebral palsy (ICP) typically presents as muscle stiffness (spasticity) and movement disorders. It results from brain injuries occurring before, during, or shortly after birth due to factors like oxygen deprivation, infections, or complications during delivery.

Types & Symptoms.
Spastic CP (75% of cases) – Stiff muscles, exaggerated reflexes.
Hemiplegia (32%) – One side of the body is affected, with the arm more impacted than the leg.
Diplegia (40%) – Both legs are more affected than the arms.
Tetraplegia (2%) – All limbs are impacted, often with significant developmental delays.
Bilateral Hemiplegia & Triplegia – Varying paralysis affecting multiple limbs.
Common complications include stiff joints, difficulty in sitting or walking, speech delays, and posture abnormalities.
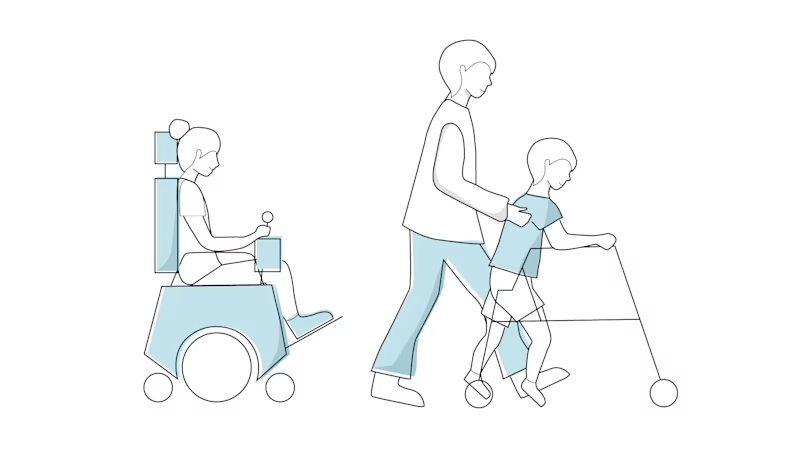
Améliorer la mobilité des enfants atteints de paralysie cérébrale
Tout d'abord, le traitement de l'infirmité motrice cérébrale dépend du type de symptômes et de la façon dont ils affectent la vie quotidienne. L'objectif de la thérapie est d'améliorer les capacités motrices et le développement cognitif de votre enfant. L'objectif est de faire en sorte que votre enfant se tienne bien droit afin de favoriser son développement ultérieur. En outre, lors de rendez-vous réguliers, la mobilité et le développement de votre enfant seront contrôlés afin de favoriser au mieux son autonomie. Les mesures préventives jouent également un rôle important pour éviter le raccourcissement des muscles, des ligaments ou des tendons et les contractures, ainsi que les positions incorrectes.
Pour la thérapie du mouvement, votre enfant sera principalement pris en charge par des physiothérapeutes et des ergothérapeutes. Des orthophonistes et des orthopédistes font également partie de l'équipe de traitement pour apporter leur soutien.
Que signifie l'infirmité motrice cérébrale pour l'avenir de votre enfant ?
De nombreux parents d'enfants atteints de paralysie cérébrale sont incertains quant à l'avenir de leur enfant. Les questions concernant la façon dont les limitations physiques affecteront le développement et donc la perspective d'une vie indépendante et active sont souvent primordiales.
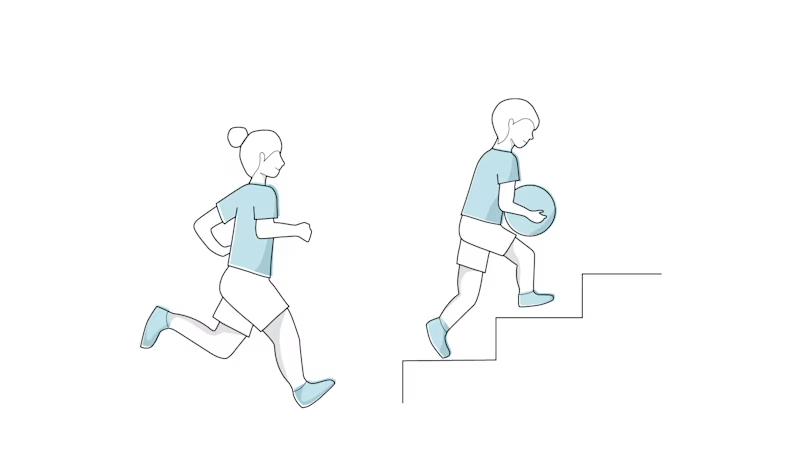
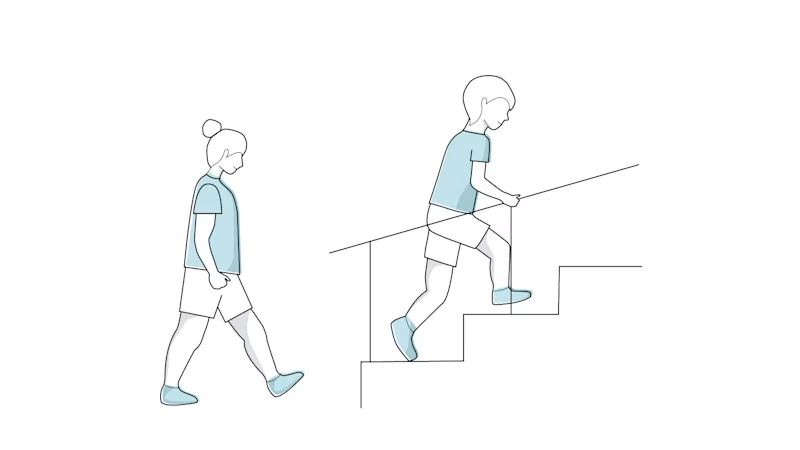
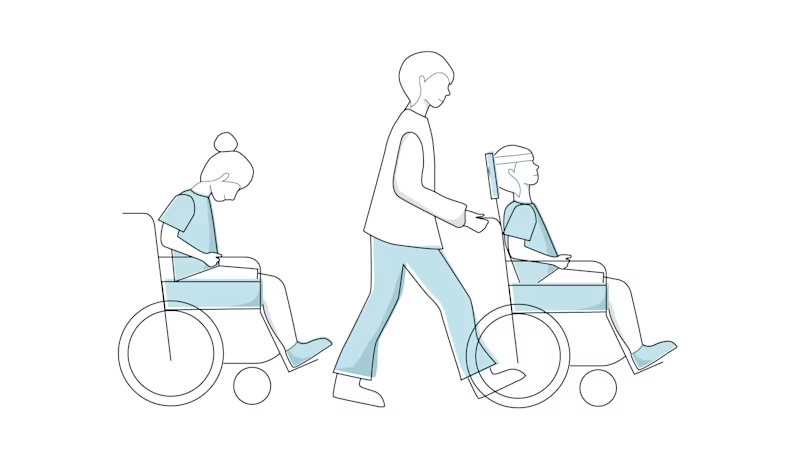
Bien que l'infirmité motrice cérébrale ne puisse être guérie et soit permanente, le maintien et l'amélioration de la mobilité sont les objectifs du traitement. Un soutien spécifique peut souvent améliorer la mobilité jusqu'à l'âge de sept ans. Plus de la moitié des enfants atteints de paralysie cérébrale peuvent marcher de manière autonome.
Par ailleurs, la présentation clinique de l'infirmité motrice cérébrale varie fortement en fonction de l'étendue de la lésion cérébrale de votre enfant. Par conséquent, certains enfants ne sont que très limités et une vie indépendante par eux-mêmes est effectivement possible

Your child’s independence.
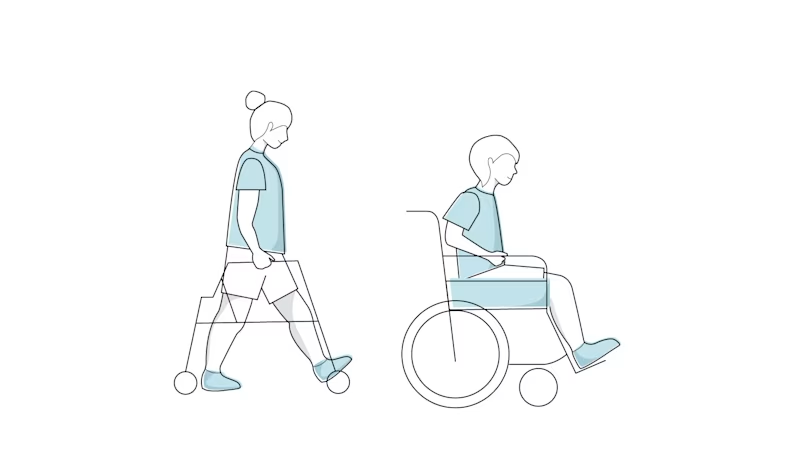
In addition, the clinical presentation of cerebral palsy varies widely depending on the extent of the injury to your child’s brain. As a result, some children are only very slightly limited, and an independent life on their own is indeed possible. If cerebral palsy is severe, it is possible that those affected will be dependent on support for the rest of their lives; however, even in this case, there are many possibilities and mobility aids to promote and shape your child’s independence and participation.
If no other serious accompanying diseases occur, cerebral palsy does not affect life expectancy.

Navigating Adolescence with CP.
Lot’s of things are changing. Including how you move!
Your teen years are a time of constant change. To your body. To what interests you and what’s important to you. You’re experiencing new feelings, looking for new kinds of friends, and starting a new part of your life.
But that can be tough when you have CP. CP can have a big impact on every part of your body, and especially on your mobility (how your body moves). Being able to move freely is more important than ever when you want to go new places, try new hobbies, and do lots more on your own.
If you’re a teen with CP, this page can help. You’ll learn a bit about what to expect at your age, and get some advice and inspiration from a real expert in what you’re going through.
Teenage years bring physical, emotional, and social challenges. For those with CP, mobility issues can affect independence, self-confidence, and participation in activities.
Key Challenges & Adaptations
Increased Spasticity & Joint Stiffness
– Growth spurts may worsen muscle tightness.
Gait Abnormalities
– Walking patterns may change, requiring updated orthotics or mobility aids.
Pain & Fatigue
– Overuse of muscles can lead to chronic pain and exhaustion.
Social Inclusion
– Teens with CP may feel different but can benefit from peer support and self-advocacy.
Maintaining Mobility & Independence
Physical & Occupational Therapy
– Adjusting treatments to accommodate growth and new physical challenges.
Assistive Devices
– Custom wheelchairs, braces, and adaptive technology for greater independence.
Mental Health Support
– Addressing self-esteem, anxiety, and social concerns through counseling and peer groups.
Encouraging independence and confidence is key to helping teens transition into adulthood successfully.
Find out what to expect — from a teen just like you!
Grownups and doctors have a lot of the answers you need when you have CP. But while they want what’s best for you, sometimes it just helps to hear it from someone your age. Someone who’s going through the same experiences and changes as you.
So to share what it’s like being a teen with CP, we asked a real expert: a teen with CP. Let’s meet her!
How to take on life’s new challenges with CP.
Moya-May has a real passion for helping others with disabilities like her. She loves to share what she’s learned about growing up with her condition, so we asked her for some real-life advice in this special video series. Keep scrolling to watch them all!
Being a teen with CP: Learning as you grow.
Being a teen can be tough for anyone. But it’s even more challenging when you’re facing a disability like CP. You want to do more on your own. And you want to feel accepted as you are.
In this video, Moya-May talks about how important that is for her too. CP doesn’t have to make you feel different, she says. It’s okay to be who you are, and to share how you’re feeling as your body changes and grows.
What to expect and how to get ready.
Everyone’s teen years are different, but there are still a lot of things that just about everyone goes through. Like wanting to know that people love and understand you.
Moya-May says that starts with being kind and patient when people ask questions about you and your CP. She loves to share how things are for her. It helps everyone understand, accept, and care for each other.

Adulthood: Long-Term Management.
While Cerebral Palsy (CP) is a non-progressive condition, its symptoms can evolve and present new challenges in adulthood due to aging, lifestyle factors, and the long-term impact of the condition on the body. Below are the most common symptoms experienced by adults with CP:
1. Motor and Mobility Issues:
Increased Muscle Stiffness and Spasticity: Worsening tightness in muscles over time. Muscle tone imbalances may lead to contractures (permanent tightening of muscles) and reduced flexibility.
Reduced Mobility: Difficulty walking or maintaining balance, increased reliance on mobility aids.
Joint and Muscle Pain: Often caused by abnormal posture, overuse, or arthritis.
Fatigue: Increased energy expenditure for routine activities due to inefficient movement patterns.
Muscle Weakness: Gradual weakening of muscles, impacting daily functions.
2. Postural Changes:
Joint Deformities: Development of contractures or scoliosis.
Poor Posture: Difficulty maintaining proper alignment while sitting or standing.
3. Speech and Swallowing Problems:
Dysarthria: Slurred or slow speech patterns.
Swallowing Difficulties (Dysphagia): Increased risk of choking or aspiration.
4. Chronic Pain:
Pain in the muscles, joints, and nerves, often due to years of abnormal muscle use and misalignment.
5. Cognitive and Mental Health Challenges:
Cognitive Decline: Some adults may experience memory or concentration difficulties.
Mental Health Concerns: Higher risk of depression, anxiety, and emotional distress.
Social Isolation: Challenges in social integration and maintaining relationships.
6. Secondary Health Issues:
Arthritis: Accelerated joint wear and tear.
Osteoporosis: Increased risk of bone fractures.
Incontinence: Bladder or bowel control issues.
Seizures: Some adults may continue to experience epileptic episodes.
7. Fatigue and Reduced Endurance & Post-Impairment Syndrome:
Daily activities may become increasingly exhausting due to the extra effort required for movement and posture control.
Post-impairment syndrome is a common condition that occurs when you max out your body's energy repeatedly. If you have CP, you may use all your energy doing certain everyday tasks, such as climbing small flights of stairs or sweeping the floor.
8. Premature Aging:
Adults with CP may experience physical aging earlier than the general population due to the strain on their muscles and joints over time.
Treatment Options for Cerebral Palsy.
While there is no cure, various treatments can help manage symptoms and improve quality of life. These include physiotherapy, occupational therapy, speech therapy, medications, assistive devices, and, in some cases, surgery. Early intervention and a personalised treatment plan are key to addressing the unique needs of each individual. Explore our site to learn more about CP, available treatment options, and resources for support and care.
Where to find support.
Your doctor is your first point of contact. Later, allied health professionals such as Physiotherapists, Orthotists, Occupational Therapists, and Speech and Language Therapists will be available to assist you if you need advice.
In addition to discussing cerebral palsy within your own family and circle of friends, networking with others in a similar situation can also be helpful.